The brain, the gut,
and the microbiome
The gut-brain-axis has been thrust into the limelight as a prominent modulator of mood. Now we are considering — what is the implication of bacteria in response to medication and metabolic side effects?
Image credit: CDC
Medications and Human Metabolism
Antipsychotic (AP) medications are the cornerstone of treatment for schizophrenia (SCZ), which is composed of typical (first-generation) and atypical (second generation) APs. However, roughly a third of patients diagnosed with SCZ are considered treatment resistant. Psychiatric patients have a higher relative risk of metabolic syndrome, a combination of cardiovascular risk factors such as dyslipidemia, hypertension, stroke and obesity, than the general population. Moreover, the prevalence of metabolic side effects, type 2 diabetes and AP-induced weight gain (AIWG), are increased with the use of APs, specifically olanzapine and clozapine. The exact mechanisms by which metabolic dysfunction occurs remain unclear.
Effects of the Gut Microbiome
A relationship by which the gut microbiota (GMB) may interact with the CNS through the gut-brain axis (GBA) has long been construed. The GBA is a complex bilateral communication network that ensures proper maintenance of the gastrointestinal homeostasis. In recent decades, studies have reported causal effects of the GMB on our behaviour and brain along with elucidating the underlying molecular mechanisms. Through evolution, the human immune system has maintained a symbiotic relationship with the microbiota. Disruption of the dynamic interaction between the two can result in profound effects on human health.
Did you know?
Psychiatric patients have a higher relative risk of metabolic syndrome, a combination of cardiovascular risk factors such as dyslipidemia, hypertension, stroke and obesity, than the general population.
The GMB has been proposed as a potential target in relation to AIWG and other metabolic dysfunction due to its ability to regulate metabolism, homeostasis, and energy balance. Studies investigating the relationship between SCZ and the GMB are limited and results reported are discrepant. The GMB holds promise to clinical intervention to improve patient symptoms.
Current Studies
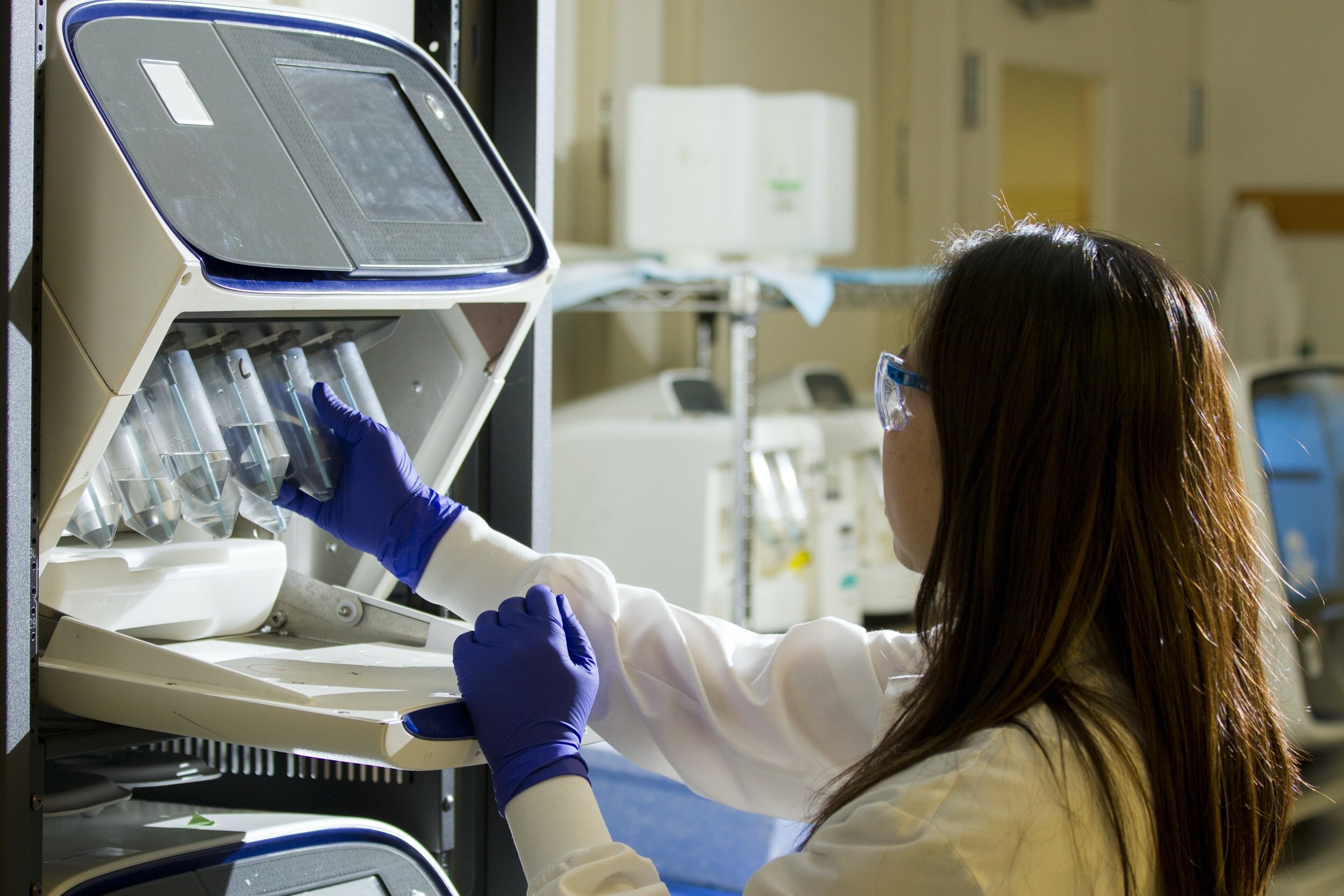
The Protocol
We are proposing a highly novel, 6-week, single arm, open-label study of 50 treatment-resistant SCZ patients to: 1) characterize the impact that clozapine initiation has on the GMB 2) identify target organisms and metabolic pathways associated with positive (i.e., symptom reduction) and negative (e.g., weight gain, gut motility) treatment outcomes. We aim to help lay the groundwork for further investigations into the role of the GMB in the development, presentation, progression and treatment of SCZ.
Figure 1 - Gorbovskaya et al., 2020
Study Completed!
The Safety, Efficacy, and Tolerability of Microbial Ecosystem Therapeutic-2 in People with Major Depression (METDA)
Microbial Ecosystem Therapeutics (MET-2) is a new treatment approach for repopulating the gut with healthy microbiota that has been developed as an alternative to fecal transplantation. This is a biological compound comprised of live microbes that normally reside in the human gut of a healthy individual. This randomized control trial with placebo will aim to measure the effects of MET-2 on symptoms of depression and anxiety using baseline and post-treatment scores to measure changes in symptom presentation. This will be accomplished by assessing subjective changes in mood and anxiety symptoms biweekly for eight weeks, from baseline, to after completion of MET-2 treatment in participants with depression, using the MADRS, HAM-A, and other mood and anxiety scales. Changes in metabolic levels and functioning before, during, and after treatment will also be assessed, along with potential correlation between early life stress (history of emotional/physical/sexual abuse, etc.), changes in Major Depressive Disorder, and response to treatment.
Selected Publications
The Gut Microbiome in Depression and Potential Benefit of Prebiotics, Probiotics and Synbiotics: A Systematic Review of Clinical Trials and Observational Studies.
Alli SR, Gorbovskaya I, Liu JCW, Kolla NJ, Brown L, Müller DJ. Int J Mol Sci. 2022 Apr 19;23(9):4494.
The Gut Microbiome in Schizophrenia and the Potential Benefits of Prebiotic and Probiotic Treatment
Liu JCW, Gorbovskaya I, Hahn MK, Müller DJ. Nutrients. 2021 Mar 31;13(4):1152.
The effect of obesity, macronutrients, fasting and nutritional status on drug-metabolizing cytochrome P450s: a systematic review of current evidence on human studies.
Zarezadeh M, Saedisomeolia A, Shekarabi M, Khorshidi M, Emami MR, Müller DJ. Eur J Nutr. 2020 Nov 3.
Investigation of the Gut Microbiome in Patients with Schizophrenia and Clozapine-Induced Weight Gain: Protocol and Clinical Characteristics of First Patient Cohorts.
Gorbovskaya I, Kanji S, Liu JCW, MacKenzie NE, Agarwal SM, Marshe VS, Sriretnakumar V, Verdu EF, Bercik P, De Palma G, Hahn MK, Müller DJ. Neuropsychobiology. 2020;79(1):5-12.
The microbiome-gut-brain axis: implications for schizophrenia and antipsychotic induced weight gain.
Kanji S, Fonseka TM, Marshe VS, Sriretnakumar V, Hahn MK, Müller DJ. Eur Arch Psychiatry Clin Neurosci. 2018 Feb;268(1):3-15.


